English for Nurses: Mastering Ascites Drainage (Paracentesis)
- sabinetorgler

- 5 days ago
- 6 min read

Table of Contents
Introduction to English for Nurses and Ascites Drainage
Understanding the Nursing Role in Paracentesis
Preparation Before Ascites Drainage
Monitoring During Paracentesis
Post-Procedure Care for Ascites Drainage
Key Nursing Safety Points
FAQ: English for Nurses on Ascites Drainage
Key Takeaway and Contact Information
Introduction to English for Nurses and Ascites Drainage
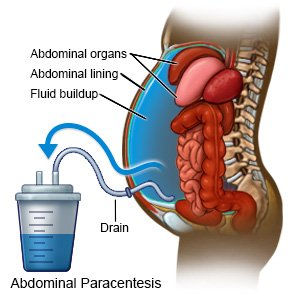
For healthcare professionals, particularly nurses, understanding complex procedures like ascites drainage is crucial. At English for Nurses, we provide tailored training that equips nurses to communicate effectively while performing clinical tasks safely. Ascites drainage, also known as paracentesis, involves removing excess fluid from the abdominal cavity, usually under sterile conditions.
This procedure is often necessary for patients experiencing severe abdominal distension, breathing difficulties, or when diagnostic testing is required for infections, liver disease, or cancer. Nurses must be familiar with both the technical and communicative aspects of the procedure to ensure patient safety and comfort. Effective communication is essential, especially when explaining the procedure to patients who may feel anxious or uncertain.
By mastering English for Nurses skills, healthcare professionals can confidently perform patient assessments, monitor vital signs, and assist in fluid removal, all while maintaining clear and compassionate communication. Whether through online courses or in-person courses, our training integrates practical examples and language guidance tailored to clinical settings.
Understanding the Nursing Role in Paracentesis
Nurses play a critical role in every stage of ascites drainage. Before the procedure, they are responsible for confirming provider orders, verifying informed consent, and performing detailed assessments, including abdominal girth, pain levels, and vital signs. Checking recent laboratory results, such as INR, platelets, and albumin levels, ensures patient safety during the procedure.
During the procedure, nurses maintain strict asepsis, monitor the patient’s blood pressure and heart rate, and provide emotional support. They observe the fluid being removed, noting colour, clarity, and volume, and label any samples for diagnostic testing. For large-volume paracentesis, nurses may assist in administering IV albumin to prevent hypotension and circulatory issues.
After the procedure, nurses continue monitoring vital signs, reassess abdominal girth and pain, and watch for complications such as infection, bleeding, or renal dysfunction. Proper documentation of fluid characteristics and patient response ensures continuity of care and helps inform future clinical decisions. By combining technical skills with effective communication, nurses embody the core principles taught in English for Nurses programmes.
Preparation Before Ascites Drainage
Preparation is key to a safe and successful paracentesis. Nurses ensure the patient’s bladder is emptied to reduce the risk of injury and position the patient in a semi-Fowler’s or upright sitting position. Equipment must be prepared using aseptic technique, and patients should receive clear instructions on what to expect during the procedure.
Patient education is a fundamental component. Explaining the purpose, steps, and sensations they might feel reassures the patient and promotes cooperation. Nurses also confirm that informed consent is documented and that all pre-procedure assessments are complete, including checking vital signs and relevant laboratory results.
English for Nurses emphasises that thorough preparation improves both patient outcomes and staff confidence. Our training programmes provide step-by-step guidance on pre-procedure protocols, ensuring nurses are prepared to manage both clinical and communicative aspects efficiently. For practical resources, nurses can access our CD language guides or pocket book guides to reinforce learning.
Monitoring During Paracentesis
Continuous monitoring during paracentesis is critical for patient safety. Nurses observe vital signs, including blood pressure, heart rate, and oxygen saturation, to detect early signs of hypotension or shock. Comfort and emotional reassurance are also essential, particularly for patients who may feel anxious about the procedure.
Observation of the fluid is another vital task. Nurses document the colour, clarity, and volume of the drained fluid, and ensure samples are sent for laboratory analysis if diagnostic testing is required. Large-volume procedures require careful monitoring to prevent complications such as circulatory collapse, particularly in patients with liver cirrhosis.
Effective communication skills, developed through English for Nurses, help nurses explain procedures in real time and respond to patient concerns. This combination of clinical skill and communication proficiency ensures procedures are performed safely, efficiently, and with minimal patient discomfort.
Post-Procedure Care for Ascites Drainage
After paracentesis, ongoing care is vital to prevent complications. Nurses apply a sterile dressing to the puncture site, monitor for leakage or infection, and continue assessing vital signs and abdominal girth. Pain management and patient comfort remain a priority during recovery.
Monitoring for complications such as hypotension, renal dysfunction, or peritonitis is essential. Patients should be educated to report dizziness, fever, or increased abdominal pain promptly. Nurses document fluid volume, appearance, and patient response to maintain accurate records and support follow-up care.
Post-procedure care also provides opportunities for language practice. Using correct terminology and clear explanations enhances patient understanding and safety. English for Nurses training programmes guide nurses through these scenarios, offering practical exercises to reinforce communication in real clinical settings.
Key Nursing Safety Points
Safety is paramount during paracentesis. Rapid fluid removal without monitoring can lead to circulatory collapse, so nurses must carefully regulate drainage speed and observe patient responses. Liver cirrhosis patients are particularly vulnerable, requiring close monitoring throughout the procedure.
Managing post-procedure fluid leakage is another important aspect. Nurses apply dressings and provide reassurance, explaining that minor leakage is common and usually not dangerous. This guidance helps reduce patient anxiety and ensures proper wound care.
Following established protocols protects both patient and clinician. English for Nurses emphasises adherence to safety standards, combining clinical competency with effective communication. Our online courses and in-person courses provide detailed safety modules, case studies, and practical simulations to build confidence and expertise.

Using S.O.A.P Notes in Ascites Drainage: English for Nurses Guidance
The S.O.A.P note is a structured method for documenting patient care, and it is essential for nurses managing ascites drainage. At English for Nurses
, we emphasise the importance of accurate documentation to support patient safety, continuity of care, and clear communication with the wider clinical team. During paracentesis, nurses use the S.O.A.P framework to organise information into Subjective, Objective, Assessment, and Plan categories.
Subjective (S) captures the patient’s perspective. For example, a patient undergoing ascites drainage may report abdominal fullness, bloating, and discomfort over the past week, along with difficulty breathing when lying flat. Patients often describe feeling heavy or uncomfortable, which can help nurses prioritise care. Recording these observations in the S.O.A.P note ensures the clinical team understands the patient’s experience and tailors interventions appropriately.
Objective (O), Assessment (A), and Plan (P) focus on measurable findings, clinical interpretation, and ongoing care strategies. Objective data may include vital signs, abdominal examination results, fluid wave detection, skin integrity, recent labs such as albumin or INR, and details of the procedure, like the volume and appearance of drained fluid. The Assessment summarises clinical reasoning, identifying ascites related to liver cirrhosis and noting potential complications such as hypotension or infection. The Plan outlines post-procedure monitoring, sterile dressing maintenance, patient education, and follow-up actions. Mastery of S.O.A.P documentation is a key skill developed in English for Nurses online courses and in-person courses, ensuring nurses can provide safe, effective care while maintaining clear communication.
FAQ: English for Nurses on Ascites Drainage
Q1: Can nurses perform ascites drainage independently?A1: Paracentesis should only be performed by trained healthcare professionals under clinical supervision. Nurses play a vital role in preparation, monitoring, and post-procedure care but do not perform the drainage independently.
Q2: What should I monitor during paracentesis?
A2: Nurses should monitor vital signs, patient comfort, and fluid characteristics. Observation for hypotension, bleeding, or infection is essential. Accurate documentation ensures patient safety and supports follow-up care.
Q3: How can English for Nurses improve my clinical communication?
A3: Our programmes focus on language skills specific to nursing scenarios, helping nurses explain procedures clearly, obtain informed consent, and provide emotional support. Resources include CD language guides and pocket book guides.
Q4: Are there resources for ongoing learning?
A4: Yes, nurses can stay updated with the latest news, research, and training opportunities on the English for Nurses blog.
Key Takeaway and Contact Information <a name="takeaway"></a>
Ascites drainage is a complex procedure requiring precision, monitoring, and communication. Nurses trained through English for Nurses gain the skills to support patients safely, provide effective education, and document procedures accurately. Mastering both clinical and language skills ensures better patient outcomes and professional confidence.
For more information on courses, practical resources, or personalised guidance, contact us directly via our contact page. Explore our online courses, in-person courses, and language guides to enhance your nursing practice today.







Comments